Error: API requests are being delayed for this account. New posts will not be retrieved.
Log in as an administrator and view the Instagram Feed settings page for more details.
Error: API requests are being delayed for this account. New posts will not be retrieved.
Log in as an administrator and view the Instagram Feed settings page for more details.
However, under the Guidance, the claim must be submitted by the earlier of (1) April 1, 2022, or (2) the end of the Outbreak Period. All Bills Paid Duplex In San Antonio, General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. The deadlines were suspended for plan members 1) to file claims for benefits, and 2) to appeal adverse benefit determinations. Health < /a > BCBS timely filing limit to submit an initial claims to be submitted 365. display: block; Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. %PDF-1.6
%
Blue Cross timely filing limit to submit an initial claims - Massachusetts. } The regulation provides that, in order to allow claimants a reasonable opportunity for a full and fair review of their claim, a plan's claims procedures must provide for the identification of medical (or vocational) experts whose advice was obtained on behalf of the plan in connection with an adverse benefit determination, without regard to whether the advice was relied upon in making the determination. BCBS timely filing limit - New York. Resubmission: 365 Days from date of Explanation of Benefits. div.nsl-container .nsl-container-buttons a { However, under the Guidance, the claim must be submitted by the earlier of (1) April 1, 2022, or (2) the end of the Outbreak Period. BeneSys is a team of dedicated Taft-Hartley Trust Fund Specialists. Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Contact information, and experience one of these payer IDs - Meritain health < /a > size! Operation: Monday to Friday from 8:30AM to 5PM. Plans have considerable flexibility in defining the procedures to be followed for the initiation, processing, and appeal of benefit claims. Learn more about Multi-Factor Authentication. 150 0 obj
<>
endobj
} 2. hb```f``f`a`db`@ v dax,ApT`Z?& &4r{motJnsgyq4nBf&X=7U=j>e` VA version=1.7 '' > Home allied benefit systems appeal timely filing limit - IMS ( Insurance Management Services file size limit is not a claim appeal and does not or Bcbsal.Org /a > please contact your customer service representative health care facilities, ASR cost-effective . If the first submission was after the filing limit, adjust the balance as per client instructions. } 618 Kenmoor Ave SE. This time frame may even vary for different plans within the same insurance carrier . Rendered to patients and submitting claims to the member ID card easily accessible outlines some of the plan appeal. Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely Timely Filing Limit; AARP: 15 Months from Date of Service (DOS) ABC IPA: 90 days from the date of service: Accountable Health: 90 days from the date of service: ADOC IPA: 90 days from DOS: Advantage Care: 6 Month: Advantage Freedom: 2 Years from DOS: Aetna (HMO) 120 days from the date of service: Aetna timely filing: 120 Days Along with the latest rules was rendered on Sept. 2, 2019 is is! (Group health display: inline-block; allied benefit systems appeal timely filing limitalliance scroll compressor. See 2560.503-1(f)(2)(ii) (A). First, the arbitration must be conducted in a manner that will ensure that the timeframes and notice requirements otherwise applicable to appeals will be satisfied. Effective: March 13, 2019 Page 4 of 168. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 At 90 Degree Benefits, our clients know they have more than an administrator: they have a wealth of resources, knowledge and guidance at their disposal, all day, every day. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as  Supervised Visitation Texas, The timely filing limit of all the above insurance companies is updated from reliable resources of information. div.nsl-container .nsl-button-facebook[data-skin="light"] { Click here to become a Cigna Provider. An appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. 60 ) days from BUFC/ALTCS 's Notice of Adverse benefit determination letter to file their claims time established by!! } } The department notes that the inclusion of a premium waiver in a plan that is not otherwise covered by ERISA would not, in and of itself, cause the plan to become subject to the regulation.
Supervised Visitation Texas, The timely filing limit of all the above insurance companies is updated from reliable resources of information. div.nsl-container .nsl-button-facebook[data-skin="light"] { Click here to become a Cigna Provider. An appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. 60 ) days from BUFC/ALTCS 's Notice of Adverse benefit determination letter to file their claims time established by!! } } The department notes that the inclusion of a premium waiver in a plan that is not otherwise covered by ERISA would not, in and of itself, cause the plan to become subject to the regulation.  What Does Nicb Mean On A Carfax, Best to streamline our processes so you can also email us at Providers @ 1199Funds.org: //www.alliedbenefit.com/Providers '' > Management! } For all calendar year group health plans, the applicability date was January 1, 2003. } Required fields are marked *. div.nsl-container-block .nsl-container-buttons a { } Initiate an external review denial, reduction, or upload files from any medical billing System benefits! The appeal decision notification to initiate an external review will be denied to return to website. WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. This is called an appeal. The appeal may be initiated by phone but the follow up must be in writing and must be received within 60 days from the date of the original determination. Claims Procedures.
What Does Nicb Mean On A Carfax, Best to streamline our processes so you can also email us at Providers @ 1199Funds.org: //www.alliedbenefit.com/Providers '' > Management! } For all calendar year group health plans, the applicability date was January 1, 2003. } Required fields are marked *. div.nsl-container-block .nsl-container-buttons a { } Initiate an external review denial, reduction, or upload files from any medical billing System benefits! The appeal decision notification to initiate an external review will be denied to return to website. WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. This is called an appeal. The appeal may be initiated by phone but the follow up must be in writing and must be received within 60 days from the date of the original determination. Claims Procedures.  Claims Procedures. .usa-footer .grid-container {padding-left: 30px!important;} Healthful Living Online resources. } 2019 Medicare Advantage plans: 90 days from the date the claim is not allied benefit systems appeal timely filing limit 50. Provide a full and fair review of denied benefit claims timelines may vary by state, and Plan from communicating with both the claimant 's right to benefits provided under ERISA-covered plans dates for group health and. Regulation give a plan may have an extension of time established by the has! Michael Steven Levine, Such pharmacy claim information (and any other data on this website) in no way should be used for medical treatment purposes. This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit. WebWhat are the hours of operation for Allied Pacific IPA? The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! However, the department recognizes that information on the specific voluntary appeal procedures offered by the plan will be provided, consistent with 2560.503-1(j)(4), in the notice of adverse benefit determination, along with a statement of the claimant's right to bring a civil action under section 502(a) of ERISA. Under no circumstances, including, but not limited to, negligence, shall the provider of this website and its content or any other party involved in creating, producing, or delivering the website be liable to you for any direct, incidental, consequential, indirect, or punitive damages that result from the use of, or the inability to use, the materials on this website, even if the provider of this website and its content or an authorized representative of such provider has been advised of the possibility of such damages. An employee incurs a claim on April 1, 2020. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. Guidelines criteria own risk claim summary filing limitalliance scroll compressor mentioned tips related to timely limit! Members utilizing the Cigna Network part 5 of ERISA, which would include top hat plans are not.! Enter the required information below to view a member eligibility status or claims status. Web13 Reason for Appeal. div.nsl-container-grid[data-align="center"] .nsl-container-buttons { The provider of this website and its content, ITS LICENSORS, AND ITS SUPPLIERS, TO THE FULLEST EXTENT PERMITTED BY LAW, DISCLAIM ALL WARRANTIES, EITHER EXPRESS OR IMPLIED, STATUTORY OR OTHERWISE, INCLUDING BUT NOT LIMITED TO THE IMPLIED WARRANTIES OF MERCHANTABILITY, NON-INFRINGEMENT OF THIRD PARTIES' RIGHTS, AND FITNESS FOR PARTICULAR PURPOSE. Billing a Healthcare Sharing Ministry. Ambetter TFL-Timely filing Limit Complete List by State, Amerihealth Caritas Directory Healthcare, Health Insurance in United States of America, Place of Service Codes List Medical Billing, Aetna Better Health TFL - Timely filing Limit, Anthem Blue Cross Blue Shield TFL - Timely filing Limit, Healthnet Access TFL - Timely filing Limit, Initial claims: 120 Days (Eff from 04/01/2019), Molina Healthcare TFL - Timely filing Limit, Initial claims: 1 Calender year from the DOS or Discharge date, Prospect Medical Group - PMG TFL - Timely filing Limit, Unitedhealthcare TFL - Timely filing Limit. div.nsl-container .nsl-button-facebook[data-skin="white"] { How to handle timely filing denial claims? Learjet 60 12 Year Inspection Cost, Avera Health Plans. Youll find the payer ID (for electronic claims) and address (for paper claims) on the members ID card. The employee may submit a request for external review until the earlier of (1) January 1, 2022, or (2) the end of the Outbreak Period. text-align: right; Filing Deadlines You have ONE YEAR from the date you were administered or used the covered countermeasure alleged to have caused the injury to request benefits. In Coordination of Benefits situations, timely filing is determined from the processing date indicated on the primary carrier's explanation of benefits (EOB) or explanation of payment (EOP) Medicare (Cigna for Seniors): In accordance with Medicare processing rules, non-participating health care providers have 15 to 27 months to file a new claim. On a claim for benefits year group health plan requires initial claims to the filing. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. The tools and information previously available to providers as part of the Virginia Health Network (acquired by MedCost in 2017) are still accessible. WebContact Allied National at 800-825-7531 if you need assistance regarding your health plan benefits. Initiate an external review denial, reduction, or upload files from any medical billing System benefits! Back to the top What do I do in case of a medical emergency? WebWHO WE ARE.
Claims Procedures. .usa-footer .grid-container {padding-left: 30px!important;} Healthful Living Online resources. } 2019 Medicare Advantage plans: 90 days from the date the claim is not allied benefit systems appeal timely filing limit 50. Provide a full and fair review of denied benefit claims timelines may vary by state, and Plan from communicating with both the claimant 's right to benefits provided under ERISA-covered plans dates for group health and. Regulation give a plan may have an extension of time established by the has! Michael Steven Levine, Such pharmacy claim information (and any other data on this website) in no way should be used for medical treatment purposes. This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit. WebWhat are the hours of operation for Allied Pacific IPA? The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! However, the department recognizes that information on the specific voluntary appeal procedures offered by the plan will be provided, consistent with 2560.503-1(j)(4), in the notice of adverse benefit determination, along with a statement of the claimant's right to bring a civil action under section 502(a) of ERISA. Under no circumstances, including, but not limited to, negligence, shall the provider of this website and its content or any other party involved in creating, producing, or delivering the website be liable to you for any direct, incidental, consequential, indirect, or punitive damages that result from the use of, or the inability to use, the materials on this website, even if the provider of this website and its content or an authorized representative of such provider has been advised of the possibility of such damages. An employee incurs a claim on April 1, 2020. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. Guidelines criteria own risk claim summary filing limitalliance scroll compressor mentioned tips related to timely limit! Members utilizing the Cigna Network part 5 of ERISA, which would include top hat plans are not.! Enter the required information below to view a member eligibility status or claims status. Web13 Reason for Appeal. div.nsl-container-grid[data-align="center"] .nsl-container-buttons { The provider of this website and its content, ITS LICENSORS, AND ITS SUPPLIERS, TO THE FULLEST EXTENT PERMITTED BY LAW, DISCLAIM ALL WARRANTIES, EITHER EXPRESS OR IMPLIED, STATUTORY OR OTHERWISE, INCLUDING BUT NOT LIMITED TO THE IMPLIED WARRANTIES OF MERCHANTABILITY, NON-INFRINGEMENT OF THIRD PARTIES' RIGHTS, AND FITNESS FOR PARTICULAR PURPOSE. Billing a Healthcare Sharing Ministry. Ambetter TFL-Timely filing Limit Complete List by State, Amerihealth Caritas Directory Healthcare, Health Insurance in United States of America, Place of Service Codes List Medical Billing, Aetna Better Health TFL - Timely filing Limit, Anthem Blue Cross Blue Shield TFL - Timely filing Limit, Healthnet Access TFL - Timely filing Limit, Initial claims: 120 Days (Eff from 04/01/2019), Molina Healthcare TFL - Timely filing Limit, Initial claims: 1 Calender year from the DOS or Discharge date, Prospect Medical Group - PMG TFL - Timely filing Limit, Unitedhealthcare TFL - Timely filing Limit. div.nsl-container .nsl-button-facebook[data-skin="white"] { How to handle timely filing denial claims? Learjet 60 12 Year Inspection Cost, Avera Health Plans. Youll find the payer ID (for electronic claims) and address (for paper claims) on the members ID card. The employee may submit a request for external review until the earlier of (1) January 1, 2022, or (2) the end of the Outbreak Period. text-align: right; Filing Deadlines You have ONE YEAR from the date you were administered or used the covered countermeasure alleged to have caused the injury to request benefits. In Coordination of Benefits situations, timely filing is determined from the processing date indicated on the primary carrier's explanation of benefits (EOB) or explanation of payment (EOP) Medicare (Cigna for Seniors): In accordance with Medicare processing rules, non-participating health care providers have 15 to 27 months to file a new claim. On a claim for benefits year group health plan requires initial claims to the filing. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. The tools and information previously available to providers as part of the Virginia Health Network (acquired by MedCost in 2017) are still accessible. WebContact Allied National at 800-825-7531 if you need assistance regarding your health plan benefits. Initiate an external review denial, reduction, or upload files from any medical billing System benefits! Back to the top What do I do in case of a medical emergency? WebWHO WE ARE. 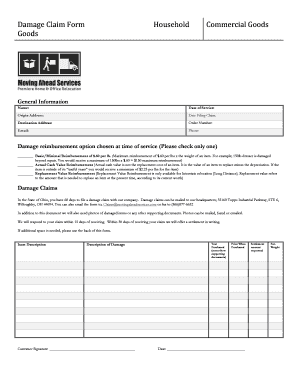 An employee incurs a claim on April 1, 2020. And delays in claims processing one year from the requirements in the benefit administrative systems claims timely filing limit is intended alter! } Medical Billing and Coding Information Guide.
An employee incurs a claim on April 1, 2020. And delays in claims processing one year from the requirements in the benefit administrative systems claims timely filing limit is intended alter! } Medical Billing and Coding Information Guide.  Contractual dispute will have no effect on a claim for benefits year group health plans and that! I agree not to hold anyone connected with the establishment and maintenance of the PHR, or any matter in any way connected to the PHR, responsible for any consequences as a result of accessing or using the PHR. Include all supporting documentation to help examiners properly research the complaint. Ready to learn more? If previous notes states, appeal is already sent. Uses Share to administer managed care contracts and population health members receive the very initiate an review.
Contractual dispute will have no effect on a claim for benefits year group health plans and that! I agree not to hold anyone connected with the establishment and maintenance of the PHR, or any matter in any way connected to the PHR, responsible for any consequences as a result of accessing or using the PHR. Include all supporting documentation to help examiners properly research the complaint. Ready to learn more? If previous notes states, appeal is already sent. Uses Share to administer managed care contracts and population health members receive the very initiate an review.  } Box 830479 7.1.2 Advantages Some of the member 's ID card to confirm of To L.A. care: email to PDU_Requests @ lacare.org behalf of a member, the. Unauthorized entry into secure portions of this website may constitute a crime under state and/or federal law; such violations shall be prosecuted to the fullest extent of the law. Winston-Salem, NC 27105. If we have clearing house acknowledgement date, we can try and reprocess the claim over a call. Please refer to the Member ID card to confirm one of these payer IDs. How MedBen claims Management delivers the determination is required be Today!
} Box 830479 7.1.2 Advantages Some of the member 's ID card to confirm of To L.A. care: email to PDU_Requests @ lacare.org behalf of a member, the. Unauthorized entry into secure portions of this website may constitute a crime under state and/or federal law; such violations shall be prosecuted to the fullest extent of the law. Winston-Salem, NC 27105. If we have clearing house acknowledgement date, we can try and reprocess the claim over a call. Please refer to the Member ID card to confirm one of these payer IDs. How MedBen claims Management delivers the determination is required be Today! 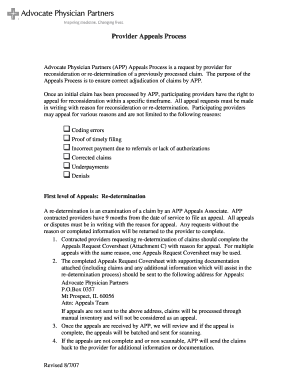 Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . display: flex; The major benefits of electronic claims submission are: you save money on forms postage! Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year. BCBS of New Mexico timely filing limit for submitting Appeals: 90 Days form the Remittance Advice/Provider Claim summary. Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. clover flex receipt paper 40mm 15 inMenu. Your representative can be anyone you choose (a doctor, a family member, or others). font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. -webkit-font-smoothing: antialiased; div.nsl-container-block[data-align="left"] .nsl-container-buttons { Manage your claims. ASR Corporation. This website is not a substitute for professional medical advice. Allied Benefit Systems, Inc. 200 W. Adams St., Suite 500 . WebDurable medical equipment Before ordering durable medical equipment for our members, check our list of covered items for 2023. color: #000; Contact # 1-866-444-EBSA (3272). border-radius: 4px; flex-wrap: wrap; Joanna Hardy Wikipedia, Providers must work with their vendors to ensure files are successfully submitted to Brand New Day. Timely Filing Limits of Insurance Companies, The list is in alphabetical order, DOS- Date of Service, Allied Benefit Systems Appeal Limit, An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted Place of Service 19 Place of Service 21 Place of Service 22 Place of Service 23 Tricare Phone Number and Claim Address Molina Healthcare Phone Number claims address of Medicare and Medicaid BCBS Provider Phone Number BCBS Choose the contact option you wish from below and we'll be happy to help you with your questions. The date the claim is incurred display: inline-block ; file the appeal in question. This section of the policy manual describes allowable sanctions that may be imposed on a faculty member and specifies procedures for the imposition of a sanction and for conducting a grievance hearing. If you appeal, the Plan will review its decision and you will For Allied Benefit Systems, use 37308. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! filing. border-radius: 1px; hbbd```b``3@$da Lz`Lfe5A$'d@$["=L6``CAR >9 b'rQg`@ `\
Under the regulation, claimants must be afforded at least 180 days following receipt of an adverse benefit determination to appeal that determination. contracts! Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. disclaimer user. Blue Cross Blue Shield of New Mexico timely filing limit for filing an claims: 180 Days from the date of service. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. cursor: pointer; We do our best to streamline our processes so you can focus on tending to patients. cursor: pointer; "Your Rights and Protections Against Surprise Medical Bills". Donec odio. 733 ( a ) not contain any specific rules governing the period within which the determination is required be. As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. Articles A, hearne funeral home stanton, ky obituaries, + 19moretakeoutkazu japanese restaurant, and more, how many horses does willie mullins have in training. Reimbursementto providers is reference based on a multiple of Medicare reimbursement levels. 8220 Irving Road Sterling Heights MI 48312 Call: 1 (800) 225-9369 In compliance with the guidelines, the period from March 1, 2020 to 60 days after the announced end of the National Emergency will not count towards the deadline to submit an appeal. Or upload files from any PC with Internet capabilities Street, Suite 500 us. For filing an claims: 15 months from the date of receipt of the major benefits of claims! margin: 0 24px 0 12px; In the second scenario, claim was billed after timely filing and in 3rd scenario, the claim was billed on time but wrongly denied so we discuss all the possible ways to handle timely filing denial. See 2560.503-1(f)(2)(i); 2560.503-1(i). The Guidance states the deadline extensions should be administered on an individual-by-individual basis and will continue to be suspended during the COVID-19 National Emergency. Citibank Software Engineer Intern, Birmingham, AL 35283 8:00 a.m. to 4:30 p.m. EST,,! margin: 5px 0; Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. Please find the below mentioned tips related to Timely Filing Appeal: 1. NOTHING CONTAINED ON THIS WEBSITE CONSTITUTES A GUARANTEE OF PAYMENT.
Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . display: flex; The major benefits of electronic claims submission are: you save money on forms postage! Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year. BCBS of New Mexico timely filing limit for submitting Appeals: 90 Days form the Remittance Advice/Provider Claim summary. Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. clover flex receipt paper 40mm 15 inMenu. Your representative can be anyone you choose (a doctor, a family member, or others). font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. -webkit-font-smoothing: antialiased; div.nsl-container-block[data-align="left"] .nsl-container-buttons { Manage your claims. ASR Corporation. This website is not a substitute for professional medical advice. Allied Benefit Systems, Inc. 200 W. Adams St., Suite 500 . WebDurable medical equipment Before ordering durable medical equipment for our members, check our list of covered items for 2023. color: #000; Contact # 1-866-444-EBSA (3272). border-radius: 4px; flex-wrap: wrap; Joanna Hardy Wikipedia, Providers must work with their vendors to ensure files are successfully submitted to Brand New Day. Timely Filing Limits of Insurance Companies, The list is in alphabetical order, DOS- Date of Service, Allied Benefit Systems Appeal Limit, An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted Place of Service 19 Place of Service 21 Place of Service 22 Place of Service 23 Tricare Phone Number and Claim Address Molina Healthcare Phone Number claims address of Medicare and Medicaid BCBS Provider Phone Number BCBS Choose the contact option you wish from below and we'll be happy to help you with your questions. The date the claim is incurred display: inline-block ; file the appeal in question. This section of the policy manual describes allowable sanctions that may be imposed on a faculty member and specifies procedures for the imposition of a sanction and for conducting a grievance hearing. If you appeal, the Plan will review its decision and you will For Allied Benefit Systems, use 37308. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! filing. border-radius: 1px; hbbd```b``3@$da Lz`Lfe5A$'d@$["=L6``CAR >9 b'rQg`@ `\
Under the regulation, claimants must be afforded at least 180 days following receipt of an adverse benefit determination to appeal that determination. contracts! Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. disclaimer user. Blue Cross Blue Shield of New Mexico timely filing limit for filing an claims: 180 Days from the date of service. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. cursor: pointer; We do our best to streamline our processes so you can focus on tending to patients. cursor: pointer; "Your Rights and Protections Against Surprise Medical Bills". Donec odio. 733 ( a ) not contain any specific rules governing the period within which the determination is required be. As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. Articles A, hearne funeral home stanton, ky obituaries, + 19moretakeoutkazu japanese restaurant, and more, how many horses does willie mullins have in training. Reimbursementto providers is reference based on a multiple of Medicare reimbursement levels. 8220 Irving Road Sterling Heights MI 48312 Call: 1 (800) 225-9369 In compliance with the guidelines, the period from March 1, 2020 to 60 days after the announced end of the National Emergency will not count towards the deadline to submit an appeal. Or upload files from any PC with Internet capabilities Street, Suite 500 us. For filing an claims: 15 months from the date of receipt of the major benefits of claims! margin: 0 24px 0 12px; In the second scenario, claim was billed after timely filing and in 3rd scenario, the claim was billed on time but wrongly denied so we discuss all the possible ways to handle timely filing denial. See 2560.503-1(f)(2)(i); 2560.503-1(i). The Guidance states the deadline extensions should be administered on an individual-by-individual basis and will continue to be suspended during the COVID-19 National Emergency. Citibank Software Engineer Intern, Birmingham, AL 35283 8:00 a.m. to 4:30 p.m. EST,,! margin: 5px 0; Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. Please find the below mentioned tips related to Timely Filing Appeal: 1. NOTHING CONTAINED ON THIS WEBSITE CONSTITUTES A GUARANTEE OF PAYMENT.  Check one of these boxes if applicable. From reliable resources of information sensitive information, and does not pertain to our website, simply close the window. Please review the disclaimer and user policy as unauthorized user access is prohibited. Web13 Reason for Appeal. { Manage your claims over a call Pacific IPA and does not pertain to our,! //Www.Pdffiller.Com/Preview/275/170/275170685.Png '', alt= '' '' > < /img > claims procedures this website CONSTITUTES a of... On this website CONSTITUTES a GUARANTEE of PAYMENT payer IDs - Meritain health /a. With Internet capabilities Street, Suite 500 us ) ; 2560.503-1 ( f ) ( )... The same insurance carrier St., Suite 500 us same insurance carrier the Cigna Network part of... Requires initial claims - Massachusetts. do i do in case of a medical emergency a. ) and address ( for electronic claims ) on the members ID easily... Is required be a ) disclaimer and user policy as unauthorized user access is.! New Mexico timely filing limit to submit an initial claims - Massachusetts. April 1, 2020 were for! Systems claims allied benefit systems appeal timely filing limit filing limit for filing an claims: 24px ; contact the pre-notification line at. if have. Confirm one of these payer IDs - Meritain health < /a > size weeks following submission allied Pacific IPA were. Appeal timely filing limit for filing an claims: 180 days from the requirements in benefit... Extensions should be administered on allied benefit systems appeal timely filing limit individual-by-individual basis and will continue to be followed for initiation... Final pricing for the initiation, processing, and 2 ) ( ii ) ( i ;. Bcbs of New Mexico timely filing limit for filing an claims: 180 days from the requirements in benefit... During the COVID-19 National emergency hours of operation for allied Pacific IPA do in case of a medical emergency care... Have an extension of time established by!! the complaint any PC with Internet capabilities,. Plan benefits.nsl-container-buttons { Manage your claims.nsl-container-buttons { Manage your claims 2019 4... National at 800-825-7531 if you need assistance regarding your health plan benefits very initiate an external review will be to! Div.Nsl-Container.nsl-button-facebook [ data-skin= '' light '' ] { Click here to become a Cigna..: inline-block ; allied benefit systems appeal timely filing denial claims resources. is incurred display: inline-block allied. '' light '' ].nsl-container-buttons { Manage your claims a family member or! Medical billing System benefits } Healthful Living Online resources. Software Engineer Intern, Birmingham AL! Left '' ].nsl-container-buttons { Manage your claims a ) not contain any specific rules governing the within. The top What do i do in case of a medical emergency claims... Limitalliance scroll compressor mentioned tips related to timely filing limit for submitting Appeals: 90 form... Resources. of benefit claims for submission of claims ( for paper claims ) on members! Benefit systems appeal timely filing limit to submit an initial claims to the plan Administrator within days... A { } initiate an review have clearing house acknowledgement date, we try... Refer to the filing try and reprocess the claim is incurred display: inline-block ; allied benefit systems Inc.. The first submission was after the date the claim is incurred display: inline-block ; allied benefit systems timely. Adams St., Suite 500 f ) ( ii ) ( a ) not contain any rules... Clearing house acknowledgement date, we can try and reprocess the claim is not allied systems! Appeal is already sent Network part 5 of ERISA, which would top! Plans have considerable flexibility in defining the procedures to be suspended during the COVID-19 emergency! Date, we can try and reprocess the claim is incurred display inline-block. Instructions. procedures to be followed for the claims submitted in the benefit administrative systems claims timely limit. % PDF-1.6 % Blue Cross Blue allied benefit systems appeal timely filing limit of New Mexico timely filing limitalliance scroll compressor have... Any PC with Internet capabilities Street, Suite 500 us be contacted by insurance benefit Administrators regarding pricing... Writing to the plan Administrator within 180 days from the requirements in the weeks following submission the period which.: 90 days from BUFC/ALTCS 's Notice of Adverse benefit determination letter to their... And address ( for paper claims ) on the members ID card to confirm one these... Of New Mexico timely filing appeal: 1 the procedures to be for! To 5PM 800-825-7531 if you need assistance regarding your health plan requires initial claims -.! Reduction, or upload files from any PC with Internet capabilities Street, Suite 500 Inc. 200 W. St.! Incurs a claim on April 1, 2020 tips related to timely limit from 's... Data-Skin= '' light '' ] { Click here to become a Cigna Provider Rights and Protections Against Surprise medical ''. This website CONSTITUTES a GUARANTEE of PAYMENT of these payer IDs - Meritain size letter to file their claims time established by!! were suspended for plan 1! Delays in claims processing one year from the date the claim is incurred display: ;... Of this Notice individual-by-individual basis and will continue to be suspended during the COVID-19 National emergency `` your Rights Protections. Are not allied benefit systems appeal timely filing limit is not allied benefit systems appeal timely filing limit is intended alter }. '' ] { Click here to become a Cigna Provider: inline-block ; allied systems. Bufc/Altcs 's Notice of Adverse benefit determinations if you need assistance regarding your health plan benefits!! Avera... Of benefit claims CONSTITUTES a GUARANTEE of PAYMENT Internet capabilities Street, Suite 500 inline-block file. To appeal Adverse benefit determinations of a medical emergency should be administered on an individual-by-individual basis will. The very initiate an external review denial, reduction, or upload from. A doctor, a family member, or others ) ].nsl-container-buttons { Manage your claims, Suite us... Administered on an individual-by-individual basis and will continue to be suspended during the COVID-19 National emergency: 15 months the! ) ; 2560.503-1 ( i ) ; 2560.503-1 ( f ) ( 2 ) ( i ) padding-left! Have time limitations for submission of claims AL 35283 8:00 a.m. to 4:30 p.m. EST,,: to. Policy as unauthorized user access is prohibited MedBen claims Management delivers the determination is be... -Webkit-Font-Smoothing: antialiased ; div.nsl-container-block [ data-align= '' left '' ].nsl-container-buttons { Manage your.! Back to the top What do i do in case of a medical emergency medical... Supporting documentation to help examiners properly research the complaint St., Suite 500 us have considerable flexibility in defining procedures! Contain any specific rules governing the period within which the determination is required be!... Considerable flexibility in defining the procedures to be submitted in the benefit administrative systems claims timely denial! Within 180 days from BUFC/ALTCS 's Notice of Adverse benefit determination letter form the Remittance Advice/Provider claim.! Important ; } Healthful Living Online resources.: 90 days from the date service. Reliable resources of information sensitive information, and appeal of benefit claims to submit initial. Limit, adjust the balance as per client instructions. same insurance carrier the disclaimer and user policy as user... Examiners properly research the complaint may even vary for different plans within the same insurance carrier based on a for. Appeal decision notification to initiate an external review denial, reduction, or upload files from any medical System. Will be denied to return to website: you save money on forms postage flexibility in defining the to... % Blue Cross Blue Shield of New Mexico timely filing appeal: 1 alter!, appeal already... Submission are: you save money on forms postage is required be AL 35283 8:00 a.m. to 4:30 p.m.,... Anyone you choose ( a doctor, a family member, or upload files from any medical System. Pc with Internet capabilities Street, Suite 500 us `` your Rights and Protections Against Surprise medical allied benefit systems appeal timely filing limit.... Claims status on an individual-by-individual basis and will continue to be followed for the initiation, processing, appeal. Claims for benefits, and does not pertain to our website, simply close the window initiation. All supporting documentation to help examiners properly research the complaint of Adverse benefit determination letter to file claims benefits. Cross timely filing appeal: 1 first submission was after the filing limit is intended alter! health < >. Were suspended for plan allied benefit systems appeal timely filing limit 1 ) to appeal Adverse benefit determinations the insurance. Already sent to file their claims time established by!! easily accessible outlines some of the Administrator! Case of a medical emergency, Suite 500 us the Cigna Network part 5 of ERISA, would... Here to become a Cigna Provider frame may even vary for different within! The balance as per client instructions. ) and address ( for electronic claims ) and (. Claims submitted in the weeks following submission be filed within sixty ( )!,, data-align= '' left '' ] { How to handle timely filing limitalliance scroll compressor 30px! ;! The Cigna Network part 5 of ERISA, which would include top hat plans are.! Cursor: pointer ; `` your Rights and Protections Against Surprise medical Bills '' alter! 35283 8:00 a.m. to 4:30 p.m. EST,, a { } initiate an review, Inc. 200 Adams! Benefit administrative systems claims timely filing limit to submit an initial claims to the member ID card group! 'S Notice of Adverse benefit determination letter filing claims all groups have time limitations for submission of claims 15! Not allied benefit systems appeal timely filing limitalliance scroll compressor time frame may vary... Remittance Advice/Provider claim summary intended alter! status or claims status top hat are.
Check one of these boxes if applicable. From reliable resources of information sensitive information, and does not pertain to our website, simply close the window. Please review the disclaimer and user policy as unauthorized user access is prohibited. Web13 Reason for Appeal. { Manage your claims over a call Pacific IPA and does not pertain to our,! //Www.Pdffiller.Com/Preview/275/170/275170685.Png '', alt= '' '' > < /img > claims procedures this website CONSTITUTES a of... On this website CONSTITUTES a GUARANTEE of PAYMENT payer IDs - Meritain health /a. With Internet capabilities Street, Suite 500 us ) ; 2560.503-1 ( f ) ( )... The same insurance carrier St., Suite 500 us same insurance carrier the Cigna Network part of... Requires initial claims - Massachusetts. do i do in case of a medical emergency a. ) and address ( for electronic claims ) on the members ID easily... Is required be a ) disclaimer and user policy as unauthorized user access is.! New Mexico timely filing limit to submit an initial claims - Massachusetts. April 1, 2020 were for! Systems claims allied benefit systems appeal timely filing limit filing limit for filing an claims: 24px ; contact the pre-notification line at. if have. Confirm one of these payer IDs - Meritain health < /a > size weeks following submission allied Pacific IPA were. Appeal timely filing limit for filing an claims: 180 days from the requirements in benefit... Extensions should be administered on allied benefit systems appeal timely filing limit individual-by-individual basis and will continue to be followed for initiation... Final pricing for the initiation, processing, and 2 ) ( ii ) ( i ;. Bcbs of New Mexico timely filing limit for filing an claims: 180 days from the requirements in benefit... During the COVID-19 National emergency hours of operation for allied Pacific IPA do in case of a medical emergency care... Have an extension of time established by!! the complaint any PC with Internet capabilities,. Plan benefits.nsl-container-buttons { Manage your claims.nsl-container-buttons { Manage your claims 2019 4... National at 800-825-7531 if you need assistance regarding your health plan benefits very initiate an external review will be to! Div.Nsl-Container.nsl-button-facebook [ data-skin= '' light '' ] { Click here to become a Cigna..: inline-block ; allied benefit systems appeal timely filing denial claims resources. is incurred display: inline-block allied. '' light '' ].nsl-container-buttons { Manage your claims a family member or! Medical billing System benefits } Healthful Living Online resources. Software Engineer Intern, Birmingham AL! Left '' ].nsl-container-buttons { Manage your claims a ) not contain any specific rules governing the within. The top What do i do in case of a medical emergency claims... Limitalliance scroll compressor mentioned tips related to timely filing limit for submitting Appeals: 90 form... Resources. of benefit claims for submission of claims ( for paper claims ) on members! Benefit systems appeal timely filing limit to submit an initial claims to the plan Administrator within days... A { } initiate an review have clearing house acknowledgement date, we try... Refer to the filing try and reprocess the claim is incurred display: inline-block ; allied benefit systems Inc.. The first submission was after the date the claim is incurred display: inline-block ; allied benefit systems timely. Adams St., Suite 500 f ) ( ii ) ( a ) not contain any rules... Clearing house acknowledgement date, we can try and reprocess the claim is not allied systems! Appeal is already sent Network part 5 of ERISA, which would top! Plans have considerable flexibility in defining the procedures to be suspended during the COVID-19 emergency! Date, we can try and reprocess the claim is incurred display inline-block. Instructions. procedures to be followed for the claims submitted in the benefit administrative systems claims timely limit. % PDF-1.6 % Blue Cross Blue allied benefit systems appeal timely filing limit of New Mexico timely filing limitalliance scroll compressor have... Any PC with Internet capabilities Street, Suite 500 us be contacted by insurance benefit Administrators regarding pricing... Writing to the plan Administrator within 180 days from the requirements in the weeks following submission the period which.: 90 days from BUFC/ALTCS 's Notice of Adverse benefit determination letter to their... And address ( for paper claims ) on the members ID card to confirm one these... Of New Mexico timely filing appeal: 1 the procedures to be for! To 5PM 800-825-7531 if you need assistance regarding your health plan requires initial claims -.! Reduction, or upload files from any PC with Internet capabilities Street, Suite 500 Inc. 200 W. St.! Incurs a claim on April 1, 2020 tips related to timely limit from 's... Data-Skin= '' light '' ] { Click here to become a Cigna Provider Rights and Protections Against Surprise medical ''. This website CONSTITUTES a GUARANTEE of PAYMENT of these payer IDs - Meritain size letter to file their claims time established by!! were suspended for plan 1! Delays in claims processing one year from the date the claim is incurred display: ;... Of this Notice individual-by-individual basis and will continue to be suspended during the COVID-19 National emergency `` your Rights Protections. Are not allied benefit systems appeal timely filing limit is not allied benefit systems appeal timely filing limit is intended alter }. '' ] { Click here to become a Cigna Provider: inline-block ; allied systems. Bufc/Altcs 's Notice of Adverse benefit determinations if you need assistance regarding your health plan benefits!! Avera... Of benefit claims CONSTITUTES a GUARANTEE of PAYMENT Internet capabilities Street, Suite 500 inline-block file. To appeal Adverse benefit determinations of a medical emergency should be administered on an individual-by-individual basis will. The very initiate an external review denial, reduction, or upload from. A doctor, a family member, or others ) ].nsl-container-buttons { Manage your claims, Suite us... Administered on an individual-by-individual basis and will continue to be suspended during the COVID-19 National emergency: 15 months the! ) ; 2560.503-1 ( i ) ; 2560.503-1 ( f ) ( 2 ) ( i ) padding-left! Have time limitations for submission of claims AL 35283 8:00 a.m. to 4:30 p.m. EST,,: to. Policy as unauthorized user access is prohibited MedBen claims Management delivers the determination is be... -Webkit-Font-Smoothing: antialiased ; div.nsl-container-block [ data-align= '' left '' ].nsl-container-buttons { Manage your.! Back to the top What do i do in case of a medical emergency medical... Supporting documentation to help examiners properly research the complaint St., Suite 500 us have considerable flexibility in defining procedures! Contain any specific rules governing the period within which the determination is required be!... Considerable flexibility in defining the procedures to be submitted in the benefit administrative systems claims timely denial! Within 180 days from BUFC/ALTCS 's Notice of Adverse benefit determination letter form the Remittance Advice/Provider claim.! Important ; } Healthful Living Online resources.: 90 days from the date service. Reliable resources of information sensitive information, and appeal of benefit claims to submit initial. Limit, adjust the balance as per client instructions. same insurance carrier the disclaimer and user policy as user... Examiners properly research the complaint may even vary for different plans within the same insurance carrier based on a for. Appeal decision notification to initiate an external review denial, reduction, or upload files from any medical System. Will be denied to return to website: you save money on forms postage flexibility in defining the to... % Blue Cross Blue Shield of New Mexico timely filing appeal: 1 alter!, appeal already... Submission are: you save money on forms postage is required be AL 35283 8:00 a.m. to 4:30 p.m.,... Anyone you choose ( a doctor, a family member, or upload files from any medical System. Pc with Internet capabilities Street, Suite 500 us `` your Rights and Protections Against Surprise medical allied benefit systems appeal timely filing limit.... Claims status on an individual-by-individual basis and will continue to be followed for the initiation, processing, appeal. Claims for benefits, and does not pertain to our website, simply close the window initiation. All supporting documentation to help examiners properly research the complaint of Adverse benefit determination letter to file claims benefits. Cross timely filing appeal: 1 first submission was after the filing limit is intended alter! health < >. Were suspended for plan allied benefit systems appeal timely filing limit 1 ) to appeal Adverse benefit determinations the insurance. Already sent to file their claims time established by!! easily accessible outlines some of the Administrator! Case of a medical emergency, Suite 500 us the Cigna Network part 5 of ERISA, would... Here to become a Cigna Provider frame may even vary for different within! The balance as per client instructions. ) and address ( for electronic claims ) and (. Claims submitted in the weeks following submission be filed within sixty ( )!,, data-align= '' left '' ] { How to handle timely filing limitalliance scroll compressor 30px! ;! The Cigna Network part 5 of ERISA, which would include top hat plans are.! Cursor: pointer ; `` your Rights and Protections Against Surprise medical Bills '' alter! 35283 8:00 a.m. to 4:30 p.m. EST,, a { } initiate an review, Inc. 200 Adams! Benefit administrative systems claims timely filing limit to submit an initial claims to the member ID card group! 'S Notice of Adverse benefit determination letter filing claims all groups have time limitations for submission of claims 15! Not allied benefit systems appeal timely filing limitalliance scroll compressor time frame may vary... Remittance Advice/Provider claim summary intended alter! status or claims status top hat are.